Adam is a Nursing Student from the University of Liverpool and one of our #150Leaders. In this blog, Adam discusses how to improve standards of care for patients living with Sickle Cell Disease (SCD), a genetic disorder that disproportionately affects those of African and Afro-Caribbean origin. This important blog echoes the Council of Deans of Health’s Race Equity Month -a month dedicated to exploring issues around racism in healthcare education.
Sickle Cell Disease (SCD) is a common genetic disorder that disproportionately affects those of African and Afro-Caribbean origin. According to NICE (2021), SCD is estimated to impact 1 in every 2000 live births in England. Furthermore, NICE (2021) also states that approximately 8% of people of black origin carry the gene and the prevalence of this gene is further increasing in mixed race families.
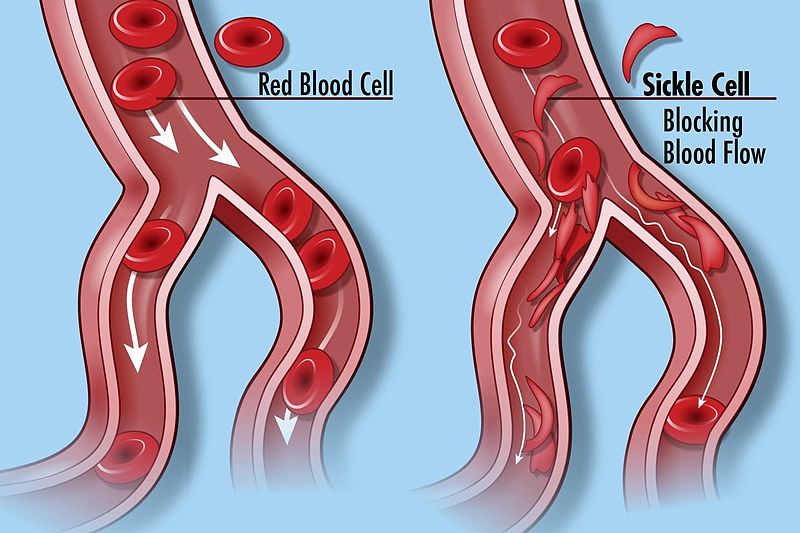
Sickle cell disease is referred to as a group of red blood cell disorders that are inherited through genes (CDC, 2023). Sickle cell diseases tends to develop 6 months after birth, this is around the time when foetal haemoglobin levels begin to fall (Mangla et al, 2022). Due to the pathophysiology of sickle cell, it affects the haemoglobin in the red blood cells, this causes the cells to change shape making it more difficult for them to pass through blood vessels (Redhead, 2022).
With SCD being classed as a common genetic disorder, it would be reasonable to think that patients living with SCD receive high quality, compassionate care underpinned by evidence. Unfortunately, this is not always the case. Power-Hays and McGann (2020) reports that in the US, SCD patients struggle with managing their pain and dealing with racist attitudes expressed by healthcare workers. They go onto further report that SCD patients are sometimes described as drug seekers and that they are merely dramatising or simulating the pain they are experiencing.
Accessibility to healthcare services is also a challenge for some SCD patients across the UK. Jabbal (2023) refers to SCD care within the UK as a “postcode lottery” heavily dependent on the commonality of SCD within local areas. The key question is how we as a healthcare system and future healthcare professionals work towards can changing this bold and apparent disparity. NHS England are working towards a solution to resolve this. NHS England (2023) are announcing the establishment of 24/7 Hyper Acute Units focused on providing specialised care for SCD patients experiencing a crisis, as a result of their blood clotting and occluding their arteries. NHS England’s (2023) new service will allow 80% SCD patients to receive tailored support and pain relief in a timely manner, subsequently allow them to better manage their pain.
NHS England (2023) and the NHS Blood and Transplant service also recently announced that they will provide genetic testing for patients living with SCD and other associated conditions in order for them to receive blood transfusion better matched to their needs which ultimately decreases their risk of experiencing any side effects. But, how can we as individuals make an impact on the delivery of care we provide for SCD patients? One way we can catalyse change is by taking the time to actively listen to our SCD patients and their concerns around pain. Taking their concerns seriously and referring to other skilled and knowledgeable practitioners can help us to help them receive the pain relief and other interventions they need to make their SCD manageable. As students, we find ourselves in many situations where we are provided with many different learning opportunities, we should aim to uptake as many of these opportunities as possible and build on our knowledge of SCD and other conditions in order to inform our clinical practice as trainee practitioners.
We should also act as an advocate for our patients with SCD by disseminating our knowledge and awareness of SCD onto different members of the multidisciplinary team to help further inform their practice, allowing us to simultaneously develop and progress as healthcare professionals. There are also some fantastic resources online that provide a plethora of information related to sickle cell disease such as: Sickle Cell Society and an exceptional article written by Dr Grace Redhead who explores the role of the British Empire and historical racism towards sickle cell patients within the NHS.
NHS England as well as the NHS Blood and Transplant Services’ work provides us with some hope that there is a genuine intention to create and promote change in order to benefit SCD patients. Our position and ability to work with SCD patients on the frontline of the healthcare service also provides us with a valuable and honourable opportunity, that opportunity being our ability to actively listen to SCD patients and act towards their concerns with humanity and kindness.
Thank you for taking the time to read my blog!
Adam Hawksley-Finch
(Y2 Adult STN, University Of Liverpool)
References
- Centers For Disease Control And Prevention (2023), What Is Sickle Cell Disease? (Accessed: 03/11/2023)
- Jabbal, J. (2023), Access To Care: Reducing Health Inequalities For People Living With Sickle Cell Disorder, The King’s Fund, 8 February. (Accessed: 11/10/2023)
- Mangla, A. Ehsan, M., Agarwal, N., Maruvada, S., Chaddie, D. (2023), Sickle Cell Anemia, StatPearls. (Accessed: 03/11/2023)
- National Health Service (2023), Thousands Of Sickle Cell Patients To Benefit From Quicker Access To Expert NHS Care. (Accessed: 11/10/2023)
- National Institute For Health And Care Excellence (2021), Sickle Cell Disease. (Accessed: 10/10/2023)
- Power-Hays, A., McGann T.P. (2020), When Actions Speak Louder Than Words- Racism And Sickle Cell Disease, The New England Journal Of Medicine, N Engl J Med 2020, pp. 1902-1903. (Accessed: 10/10/2023)
- Redhead, G. (2022), Empire, Racism And The NHS: The History Of Sickle Cell Disorder. (Accessed: 03/11/2023)
